Many, many women will deal with a condition known as uterine fibroids at some point in their lives.
But what exactly are these uterine fibroids?
They are non-cancerous growths that develop in the uterus and can be a source of perplexity and cause uncomfortable side effects for women.
In this article, we will discuss this common condition affecting many of those with a uterus: its causes, signs and symptoms, diagnoses, treatment options, and more.
Table of Contents
ToggleUnderstanding Uterine Fibroids
The idea of tumors sounds scary, but uterine fibroids are tumors of the benign variety, which means they are non-cancerous.
These exist in the muscle layer of your uterus and are medically known as leiomyomas.[1]
Uterine fibroids can come in all different shapes and sizes. Many are so small that you won’t even notice.
However, others can form large masses, which can potentially distort the shape of your uterus.
Symptoms of uterine fibroids may include:
- Pelvic pain
- Heavy menstrual bleeding
- Pressure on the bladder
Let’s learn about what causes these benign tumors to appear:
Causes and Risk Factors
The exact cause of uterine fibroids remains unclear. However, there are a few key factors that contribute to their development [2]:
1. Genetic Predisposition. Many health conditions run in families, and uterine fibroids are no exception. If a family member suffers from this ailment, it’s possible that you might as well.
2. Hormonal Influence. Changes in progesterone and estrogen levels in your body can make the uterus more prone to form fibroids. That’s why fibroids will often appear during your reproductive years when hormone levels regularly change.
3. Other Contributing Factors. There are a few other common factors that might make you more prone to develop fibroids, including:
- Obesity [3]
- Vitamin D deficiency [4]
- Being African American [5]
Now that you are aware of the causes of uterine fibroids, we will discuss the 3 types: submucosal, intramural, and subserosal.
Types of Uterine Fibroids
Uterine fibroids are classified by the areas in which they develop[6].
Let’s break down the types:
1. Submucosal Fibroids. These fibroids develop inside the uterine cavity. These fibroids in particular can disrupt your menstrual flow and may cause heavy bleeding.
2. Intramural Fibroids. These fibroids develop in the uterine wall. They might make your uterus feel bulkier than usual.
3. Subserosal Fibroids. These fibroids form on the outer surface of the uterus. These can cause an annoying pressure on your bladder.
However, those who suffer from uterine fibroids may not have just one type. And some uterine fibroids may not cause noticeable symptoms.
But that doesn’t mean they won’t impact your health. It is important to check in with your doctor regularly and be on the lookout for uterine fibroids.
There are a number of signs and symptoms that stem from uterine fibroids. We’ll break these down in the following section.
Common Symptoms and Signs
Those who suffer from uterine fibroids may experience the following[7]:
1. Pelvic Pain and Pressure. Pelvic pain can stem from a variety of issues, but uterine fibroids can be a common cause. Fibroids can also cause pressure, which may cause further discomfort, sometimes to the point of impacting your day-to-day activity.
2. Heavy Menstrual Bleeding. Uterine fibroids can cause heavy bleeding during your period. The fibroids can disrupt your menstrual flow and cause irregular periods.
3. Frequent Urination. The pressure from uterine fibroids can put a squeeze on your bladder, which may cause you to go to the bathroom more often.
4. Back Aches or Leg Pains. Sometimes the placement of fibroids can impact the nerves in the areas, causing back aches or leg pains.
5. Reproductive Challenges. Uterine fibroids can present hurdles for those trying to get pregnant. They can cause:
- Fertility issues
- Recurrent miscarriages
- Complications during pregnancy
As you can imagine, many of these symptoms can cause disruptions in your day-to-day life.
In the next section, we’ll discuss some of the most common issues for those suffering from uterine fibroids.

Impact on Daily Life
Living with uterine fibroids isn’t always easy. Besides the physical discomfort, they can throw a curveball into your daily routine.
There are several ways that uterine fibroids can impact your daily life, such as:
1. Disrupted Sleep
Uterine pain can leave one tossing and turning all night. Fibroids can disrupt sleep [8], which then makes you tired and irritable during the day.
2. Work and Productivity
Persistent pelvic pain can make it difficult to focus at work, hindering focus and performance[9]. It can lead to missed days or decreased efficiency in the workplace.
3. Intimacy
Uterine fibroids can disrupt your sex life. Feeling uncomfortable or in pain can easily put a damper on intimacy[10].
This can also impact other forms of social interaction, as one may need to manage symptoms versus engaging in social outings.
4. Emotional Well-being
Living with the uncertainties of uterine fibroids can take a toll on your mental health [11]. When dealing with symptoms, you might feel:
- Anxiety
- Frustration
- Isolation
If you are dealing with uterine fibroids, It is important to seek emotional support to manage these challenges.
If you are dealing with the difficult health effects of uterine fibroids, getting a proper diagnosis is the first step to conquering the issue.
Read on to learn more about diagnosing uterine fibroids.
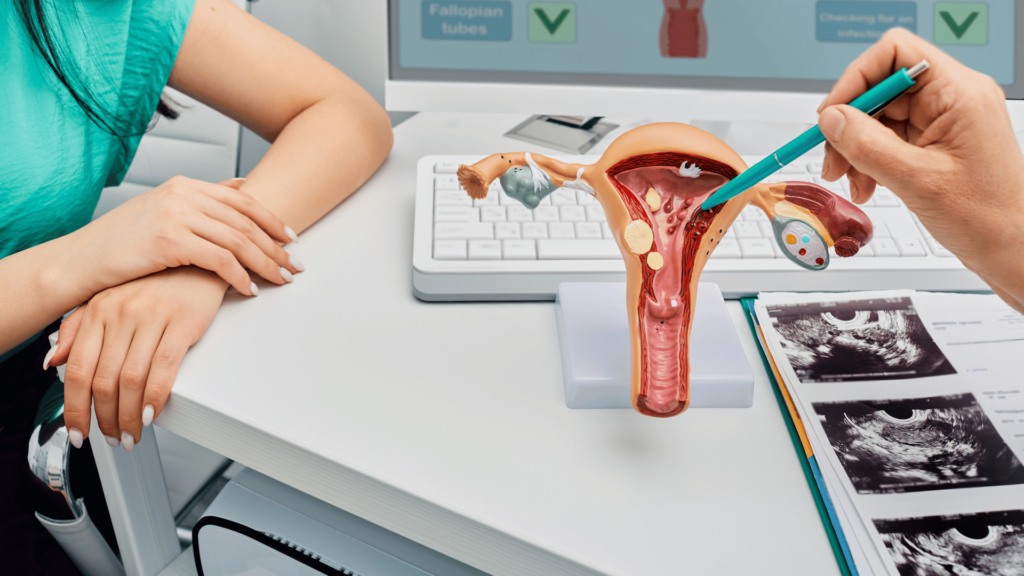
Diagnosis and Medical Evaluation
Perhaps you suspect that you or a loved one are suffering from uterine fibroids.
It’s essential to consult a medical professional to rule out other conditions and find the best treatment plan for you.
When working with your doctor, they might perform the following tests to check for uterine fibroids:
1. Pelvic Exam and Imaging
Doctors have numerous tools and procedures to determine the fibroids’ size, location, and characteristics. But oftentimes the very first step toward diagnosing uterine fibroids is a pelvic exam. Your doctor may use imaging techniques such as ultrasounds or MRIs to reach a diagnosis[12].
2. Hysteroscopy and Biopsy
In some cases, your doctor may recommend a more direct examination through hysteroscopy [13]. This procedure involves a thin, lighted tube used to observe the interior of the uterus. Biopsy, though less common, can provide further insight into the nature of the growths.
Importance of Early Detection
The sooner a medical professional can provide a uterine fibroids diagnosis, the better. Early detection can prevent complications and result in an effective treatment plan.
Regular gynecological check-ups and paying attention to changes in your body are your first line of defense.
The Personalized Treatment Plan
Once the diagnostic results are in, your doctor can create a personalized treatment for your specific situation. It’s all about finding the most effective strategies to manage and, if necessary, remove the fibroids.
No two fibroid stories are the same, and treatment is not one-size-fits-all!
Once you have your diagnosis, you’ll want to explore all of the treatment options available and find the best fit for you.
In this next section, we will talk about some of these treatment options.
Treatment Options
Uterine fibroids can be uncomfortable and painful for many women.
However, there are a number of treatment options that can provide relief.
Let’s explore the various avenues for tackling uterine fibroids:
1. Medications for Symptom Management
To ease symptoms like heavy bleeding and pelvic pain, your doctor might prescribe medications. Hormonal therapies, such as birth control pills or hormone-releasing IUDs, can regulate menstrual cycles [14].
These treatments can also relieve discomfort associated with uterine fibroids.
2. Non-Invasive Procedures: Interventional Radiologist
An interventional radiologist plays a crucial role, particularly in non-invasive procedures. For those seeking non-invasive procedures, uterine artery embolization (UAE) is emerging as a viable alternative [15].
These approaches aim to shrink or eliminate fibroids without major surgery. During this procedure, the specialist uses imaging guidance to navigate and deliver targeted interventions.
3. Surgical Interventions
In cases where fibroids cause severe symptoms or fertility issues, doctors may recommend the following surgical interventions [16]:
- Myomectomy – removing the fibroids
- Hysterectomy – removing the uterus
These decisions are often based on your health goals and preferences.
4. Alternative and Complementary Therapies
Beyond conventional treatments, the following alternative therapies may offer relief to some women:
- Acupuncture [17]
- Dietary supplements [18]
- Herbal remedies [19]
Consult with your doctor to ensure the efficacy and safety of these therapies.
In addition to treatment options, there are some lifestyle changes you can implement if you are suffering from uterine fibroids. We will discuss some of these recommended changes next in this article.
Lifestyle Changes for Management
As we’ve learned, dealing with uterine fibroids can be incredibly debilitating.
This condition can impact many parts and pieces of your event day. But there are ways to reduce its effects!
Both medical treatments and lifestyle changes can alleviate the symptoms of uterine fibroids.
Lifestyle changes for uterine fibroids management include:
1. Healthy Diet
A healthy diet rich in whole grains, vegetables, and fruits can contribute to well-being [20]. While there is no magic diet that makes fibroids disappear, choosing nutrient-rich foods can help improve symptoms.
2. Regular Exercise
Engaging in regular physical activity promotes general health and can also help manage fibroid-related symptoms [21]. Exercise may assist in maintaining a healthy weight, reducing inflammation, and managing stress, which can also reduce symptoms.
3. Stress Management
Finding effective stress management techniques is crucial when dealing with uterine fibroids. Keeping your stress levels in check can positively impact fibroid symptoms [22].
Some recommendations for stress management include:
- Deep breaths
- Meditation
- Yoga
- Indulging in other activities that bring you joy
Your mental well-being matters, and finding stress-reducing activities that suit your style is key.
4. Adequate Sleep
Quality sleep is essential for health[23]. Good sleep hygiene practices can contribute to better sleep, which also aids in managing fatigue and irritability associated with uterine fibroids. It is essential to build a solid sleep routine.
5. Limiting Alcohol and Caffeine
It can be nice to enjoy a good cup of coffee in the morning or a glass of wine at the end of the day, and moderate consumption of alcohol and caffeine is generally acceptable.
But avoid overdoing it if you suffer from uterine fibroids! These substances can potentially influence hormonal balance[24] and exacerbate symptoms.
Much like finding a treatment plan that works, living well with uterine fibroids is about finding the lifestyle rhythm that works for you.
Embrace the little changes and make them a part of your routine. With a mix of lifestyle adjustments, you can see a vast improvement in uterine fibroid symptoms.
Now, let’s talk about managing fibroids and fertility.
Managing Fibroids and Fertility
As we mentioned earlier in this article, uterine fibroids can have an impact on fertility.
Learning more about its effects can help you plan if you suffer from this condition and would like to start a family at some point.
Read on to learn more about fertility, pregnancy, and uterine fibroids:
Risks During Pregnancy
While pregnancy with uterine fibroids is generally manageable, it may pose certain risks [25]. Complications include:
- A higher likelihood of cesarean delivery (“C-section”)
- Breech birth
- Preterm delivery
Preconception Planning
If you suffer from uterine fibroids, and you are planning to start a family, a bit of preconception planning can go a long way.
This involves:
- Discussing your fertility goals with your doctor [26]
- Evaluating the impact of fibroids
- Determining proactive steps to take (if applicable to your situation)
Fibroid Management During Pregnancy
If you’re dealing with uterine fibroids while already on your pregnancy journey, regular check-ins with your healthcare team become crucial.
Monitoring the growth and impact of fibroids during pregnancy ensures that any necessary interventions can be implemented on time [27].
Timing of Fibroid Removal
If you’re planning a pregnancy and fibroids are a known factor, discuss the timing of any necessary fibroid removal with your doctor.
Some interventions, like myomectomy [28], can be performed before conception. This helps optimize the chances of a healthy pregnancy.
Embracing the Pregnancy Journey
When navigating pregnancy with uterine fibroids, it is essential to work closely with your doctor during the process.
The following proactive measures create a supportive environment for a healthy and positive pregnancy experience:
- Open communication
- Regular check-ups [29]
- Addressing any concerns promptly
If you decide to give birth while experiencing uterine fibroids, being equipped with this knowledge and working with a communicative medical professional will be the best course of action.
Debunking Common Myths
The exact cause of uterine fibroids is indeed unclear, so this condition can seem mysterious.
However, there are many myths about this condition that should be corrected.
Here are some of those myths – and the actual truth about uterine fibroids:
Myth 1: Uterine Fibroids Only Affect Older Women
Reality: Uterine fibroids don’t discriminate based on age. While they are more common in women aged 30 and above, they can develop at any reproductive age [30].
Younger women can also experience uterine fibroids, and their impact can vary.
Myth 2: Uterine Fibroids Always Cause Symptoms
Reality: Not all uterine fibroids come with a side of noticeable symptoms [31]. Some women may have uterine fibroids without even realizing it. Fibroids can be present without causing:
- Pain
- Heavy bleeding
- Other visible signs
Myth 3: Fibroids Always Lead to Hysterectomy
Reality: Hysterectomy, the removal of the uterus, is one treatment option. However, it’s not the only one.
Many women with fibroids can explore alternative treatments like:
- Myomectomy (removing the fibroids while preserving the uterus)
- Non-invasive procedures, like uterine artery embolization [32]
Myth 4: Pregnancy is Impossible with Uterine Fibroids
Reality: Uterine fibroids can sometimes affect fertility. However, many women with fibroids can conceive and have healthy pregnancies [33].
Early medical guidance from your doctor can help manage potential challenges during conception and pregnancy.
Myth 5: Uterine Fibroids Always Require Treatment
Reality: Not all uterine fibroids cases require immediate intervention [34]. Small, symptom-free fibroids can be monitored without active treatment, particularly if they’re not affecting your daily life.
Treatment decisions depend on factors like size, location, and symptoms of the fibroids.
Myth 6: Uterine Fibroids Are Always Cancerous
Reality: Fibroids are almost always non-cancerous, known as benign tumors.
While extremely rare, some types of uterine cancers can mimic fibroid symptoms [35]. Diagnostic procedures can help differentiate between fibroids and potential cancerous growths.
Myth 7: Uterine Fibroids Are Caused by Stress Alone
Reality: The exact cause of fibroids remains unclear. Stress is just one potential factor among many [36].
Hormonal, genetic, and environmental factors also play roles in fibroid development. Stress management can benefit well-being, but stress isn’t the sole cause of fibroids.
Myth 8: Uterine Fibroids Always Grow Back After Treatment
Reality: The recurrence of fibroids after treatment depends on a variety of factors, including the type of treatment received [37]. The success in preventing regrowth can vary in surgical procedures and non-invasive treatments.
It is important to not only raise awareness of this condition and its symptoms but also to understand myth versus fact.
Armed with this knowledge, those who experience uterine fibroids can better understand their condition sooner and seek the help that they need.
Conclusion
As we conclude this article about uterine fibroids, it’s clear that knowledge is a key pillar in navigating this journey.
Uterine fibroids can cause a tremendous amount of discomfort and greatly impact the day-to-day lives of women everywhere.
Fortunately, while its cause is still unclear, there are several solutions out there to manage the symptoms of this condition.
Understanding the nuances of uterine fibroids empowers you to make informed decisions about your health.
Your journey with uterine fibroids is unique, and your care plan should be too. Embrace personalized care, and seek support from your doctor.
If you or a loved one are experiencing symptoms of uterine fibroids, interventional radiology may be a solution for you. At [Imaging and Interventional Radiology], our team of dedicated experts maintains a patient-focused approach, providing high-quality care with compassion and expertise.
You shouldn’t have to suffer. Take the first step towards relief and improving your everyday well-being. Contact Imaging and Interventional Radiology today!
Resources
1. https://www.nhs.uk/conditions/fibroids/
2. https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/symptoms-causes/syc-20354288
3. Shikora SA, Niloff JM, Bistrian BR, Forse RA, Blackburn GL. Relationship between obesity and uterine leiomyomata. Nutrition. 1991 Jul-Aug;7(4):251-5. PMID: 1802214.
4. Hajhashemi M, Ansari M, Haghollahi F, Eslami B. The effect of vitamin D supplementation on the size of uterine leiomyoma in women with vitamin D deficiency. Caspian J Intern Med. 2019 Spring;10(2):125-131. doi: 10.22088/cjim.10.2.125. PMID: 31363390; PMCID: PMC6619469.
5. Eltoukhi HM, Modi MN, Weston M, Armstrong AY, Stewart EA. The health disparities of uterine fibroid tumors for African American women: a public health issue. Am J Obstet Gynecol. 2014 Mar;210(3):194-9. doi: 10.1016/j.ajog.2013.08.008. Epub 2013 Aug 11. PMID: 23942040; PMCID: PMC3874080.
6.https://www.nichd.nih.gov/health/topics/uterine/conditioninfo
7. https://www.nichd.nih.gov/health/topics/uterine/conditioninfo/symptoms
8. https://www.fertstert.org/article/S0015-0282(02)04539-9/fulltext
9. Hunsche E, Rakov V, Scippa K, Witherspoon B, McKain L. The Burden of Uterine Fibroids from the Perspective of US Women Participating in Open-Ended Interviews. Womens Health Rep (New Rochelle). 2022 Mar 4;3(1):286-296. doi: 10.1089/whr.2021.0086. PMID: 35415708; PMCID: PMC8994433.
10. Don EE, Mijatovic V, Huirne JAF. Infertility in patients with uterine fibroids: a debate about the hypothetical mechanisms. Hum Reprod. 2023 Nov 2;38(11):2045-2054. doi: 10.1093/humrep/dead194. PMID: 37771247; PMCID: PMC10628498.
11. Chiuve SE, Huisingh C, Petruski-Ivleva N, Owens C, Kuohung W, Wise LA. Uterine fibroids and incidence of depression, anxiety and self-directed violence: a cohort study. J Epidemiol Community Health. 2022 Jan;76(1):92-99. doi: 10.1136/jech-2020-214565. Epub 2021 Jul 22. PMID: 34301795; PMCID: PMC8666805.
12. Palheta MS, Medeiros FDC, Severiano ARG. Reporting of uterine fibroids on ultrasound examinations: an illustrated report template focused on surgical planning. Radiol Bras. 2023 Mar-Apr;56(2):86-94. doi: 10.1590/0100-3984.2022.0048. PMID: 37168038; PMCID: PMC10165971.
13. Emanuel MH. Hysteroscopy and the treatment of uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2015 Oct;29(7):920-9. doi: 10.1016/j.bpobgyn.2015.03.014. Epub 2015 Apr 1. PMID: 25937553.
14. Moroni R, Vieira C, Ferriani R, Candido-Dos-Reis F, Brito L. Pharmacological treatment of uterine fibroids. Ann Med Health Sci Res. 2014 Sep;4(Suppl 3):S185-92. doi: 10.4103/2141-9248.141955. PMID: 25364587; PMCID: PMC4212375.
15. https://www.acog.org/womens-health/faqs/uterine-artery-embolization
16. https://www.nhs.uk/conditions/fibroids/treatment/
17. https://www.frontiersin.org/articles/10.3389/fmed.2023.1268220
18. Szydłowska I, Nawrocka-Rutkowska J, Brodowska A, Marciniak A, Starczewski A, Szczuko M. Dietary Natural Compounds and Vitamins as Potential Cofactors in Uterine Fibroids Growth and Development. Nutrients. 2022 Feb 9;14(4):734. doi: 10.3390/nu14040734. PMID: 35215384; PMCID: PMC8880543.
19. https://www.frontiersin.org/articles/10.3389/fphar.2022.878407/full
20. Tinelli A, Vinciguerra M, Malvasi A, Andjić M, Babović I, Sparić R. Uterine Fibroids and Diet. Int J Environ Res Public Health. 2021 Jan 25;18(3):1066. doi: 10.3390/ijerph18031066. PMID: 33504114; PMCID: PMC7908561.
21. Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. Association of physical activity with development of uterine leiomyoma. Am J Epidemiol. 2007 Jan 15;165(2):157-63. doi: 10.1093/aje/kwj363. Epub 2006 Nov 7. PMID: 17090618.
22. Qin H, Lin Z, Vásquez E, Xu L. The association between chronic psychological stress and uterine fibroids risk: A meta-analysis of observational studies. Stress Health. 2019 Dec;35(5):585-594. doi: 10.1002/smi.2895. Epub 2019 Sep 5. PMID: 31452302.
23. https://newsinhealth.nih.gov/2021/04/good-sleep-good-health
24. Rachdaoui N, Sarkar DK. Effects of alcohol on the endocrine system. Endocrinol Metab Clin North Am. 2013 Sep;42(3):593-615. doi: 10.1016/j.ecl.2013.05.008. PMID: 24011889; PMCID: PMC3767933.
25. https://www.nhs.uk/conditions/fibroids/complications/
27. Lee HJ, Norwitz ER, Shaw J. Contemporary management of fibroids in pregnancy. Rev Obstet Gynecol. 2010 Winter;3(1):20-7. PMID: 20508779; PMCID: PMC2876319.
28. https://www.sciencedirect.com/science/article/abs/pii/S0301211520305303
29. https://newsinhealth.nih.gov/2021/04/pregnancy-check-ups
30. https://www.sciencedirect.com/science/article/abs/pii/S1083318820304125
31.https://www.msdmanuals.com/professional/gynecology-and-obstetrics/uterine-fibroids/uterine-fibroids
32. Szkodziak P, Szkodziak F, Trzeciak K, Czuczwar P. Minimally invasive procedures in the management of uterine fibroids. Prz Menopauzalny. 2017 Dec;16(4):122-125. doi: 10.5114/pm.2017.72756. Epub 2017 Dec 30. PMID: 29483853; PMCID: PMC5824681.
34. https://www.health.harvard.edu/womens-health/what_to_do_about_fibroids
35. https://www.cancer.org.au/cancer-information/types-of-cancer/uterine-cancer
36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2906657/
37. Kramer KJ, Ottum S, Gonullu D, Bell C, Ozbeki H, Berman JM, Recanati MA. Reoperation rates for recurrence of fibroids after abdominal myomectomy in women with large uterus. PLoS One. 2021 Dec 9;16(12):e0261085. doi: 10.1371/journal.pone.0261085. PMID: 34882735; PMCID: PMC8659682.

